Common Conditions
Pars Fracture (Spondylolysis)
Dr Young has a special interest in pars fractures and other causes of adolescent low back pain. He is a medical director of a dedicated adolescent spine clinic (Pars and Adolescent Spine Clinic) and works in collaboration with the University of Queensland, Departments of Physiotherapy and Medicine.
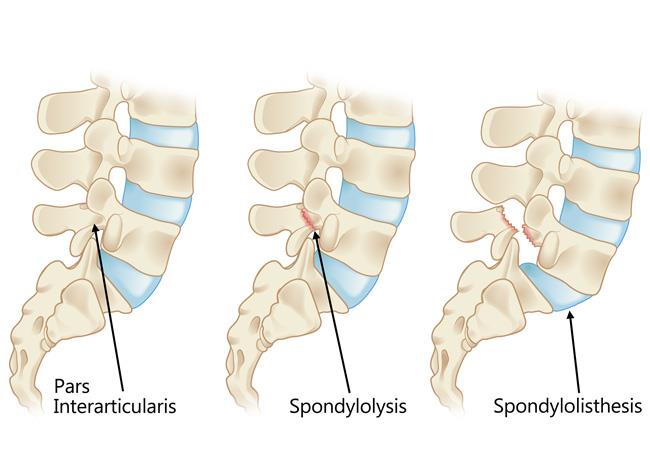
Pars stress fractures, also known as spondylolysis, are bone stress overload injuries of the pars interarticularis, a thin segment of bone that connects the upper and lower facet joints between the vertebrae. These injuries start as bone stress and progress to an incomplete then complete fracture, which may not heal. These fractures are typically seen in the lower back (lumbar spine) and are a frequent cause of back pain in young athletes. They often occur due to repetitive stress or overuse, particularly in activities that involve extension or rotation of the spine. Pars stress fractures are the commonest adolescent overuse injury and the commonest cause of adolescent low back pain. They rarely occur over the age of 20.
The practitioners at Qspine have created a unique world first “Pars Clinic” due to the high numbers of these fractures.
What causes pars stress fractures?
Pars stress fractures typically result from repetitive stress on the spine. Common causes include:
- Sporting overload: This is a major risk factor. Activities such as gymnastics, cricket, tennis, and all ball sports, which involve repeated spinal extension, twisting, or hyperextension, can put excessive stress on the pars interarticularis.
- Growth spurts: Adolescents going through rapid growth may have weaker bone structures, making them more susceptible to fractures.
- Poor biomechanics: Improper movement patterns or posture during physical activities possibly can increase strain on the pars interarticularis.
Common symptoms of pars stress fractures
The symptoms of pars stress fractures can vary in severity but often include:
- Lower back pain: Pain is typically dull or aching and worsens with activity, especially activities involving spinal extension or twisting.
- Localized tenderness: The area around the fracture may feel tender when touched.
- Muscle tightness: Tightness in the hamstrings or lower back muscles is common.
- Pain that improves with rest: Symptoms may decrease during periods of inactivity.
Diagnosis of pars stress fractures
The diagnosis of a pars stress fracture should be considered in any athlete with low back pain lasting more than a few weeks. Initially the specialist undertakes a clinical evaluation focused on the lower back, asking about symptoms, activity levels, and any history of back injury. A physical exam should include movements that stress the lower spine to reproduce pain.
Imaging tests are essential to confirm the diagnosis and to exclude other causes:
- MRI scans are now the gold standard for detecting early stress reactions or fracture well before a fracture becomes visible on X-ray.
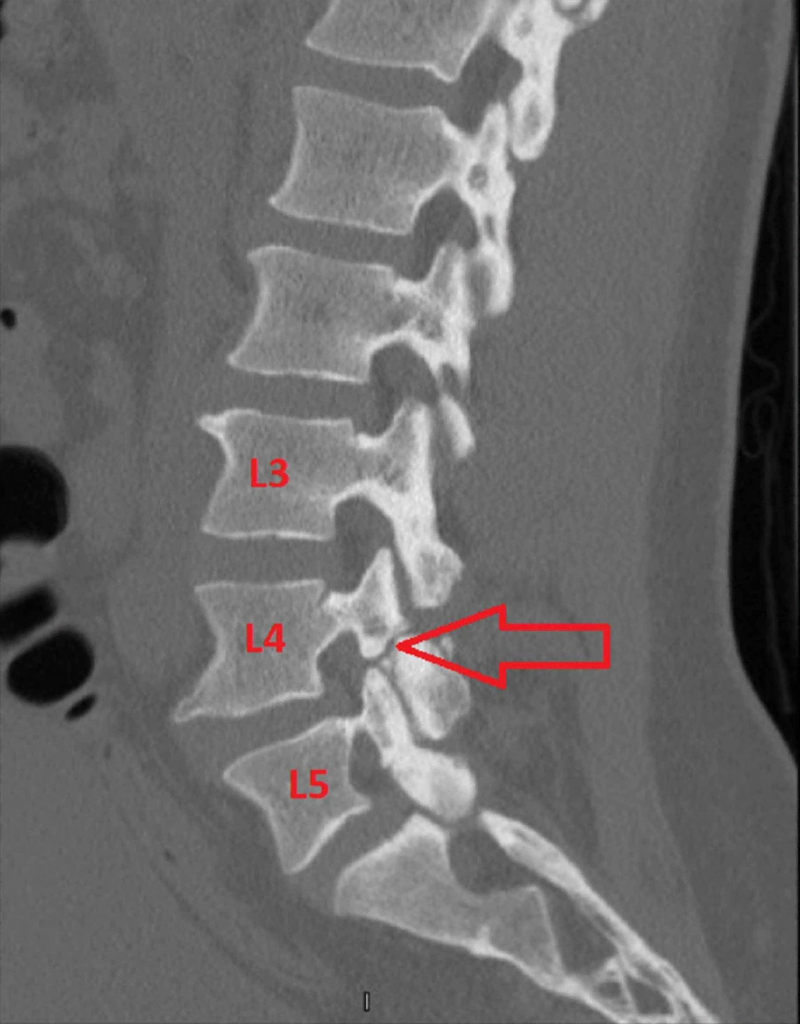
- CT scans may occasionally be required to provide a more detailed view of the bone structure and to grade the fracture.
- Nuclear medicine bone scanning is rarely required for the diagnosis and monitoring of these injuries and requires the use of ionising radiation.
- X-rays are almost never required to diagnose pars fractures is now superseded by advanced imaging protocols. However, a single standing lateral lumbar X-ray may sometimes be used to diagnose or measure a spondylolisthesis.
Early diagnosis is important to guide treatment and prevent progression to complete fracture, a pars interarticularis fracture non-union and potentially spondylolisthesis.
Management of pars stress fractures
Treatment for pars stress fractures focuses on pain relief, healing, and preventing further injury. Typically, these fractures can heal in 3-6 months. Common approaches include:
- Rest and activity modification:
— A period of rest from high-impact activities or risky activities is typically recommended.
— Bracing: In some cases, a back brace may be used to stabilize the spine and reduce stress on the fracture during healing. - Physical therapy: Exercises to strengthen the core and lower back muscles, improve flexibility, and correct movement patterns can help support the spine and prevent future injuries.
- Gradual return to activity: Once healing is confirmed, a gradual return to physical activity, under the guidance of a healthcare professional, is recommended.
- Surgical intervention: Surgery is very rarely needed but may be considered in cases of severe or painful non-healing fractures, particularly if instability or nerve compression occurs.

