Common Conditions
Discogenic pain
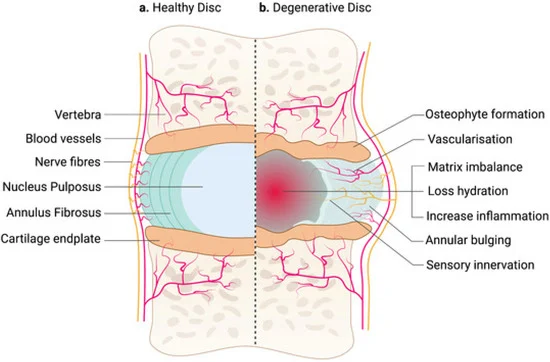
Discogenic pain refers to pain originating from one or more intervertebral discs in the spine. These discs help spinal motion and provide shock absorption between vertebrae. With ageing or repetitive injury, a disc can become damaged or degenerate, leading to inflammation and pain. Discogenic pain is often felt in the lower back or neck and may radiate to other areas, such as the hips, buttocks, or shoulders.
What causes discogenic pain?
The primary causes of discogenic (axial) pain include:
- Degeneration: Age-related wear and tear can lead to disc degeneration, reducing the discs ability to absorb shock. Some degenerate discs develop Modic changes or annular tears – both conditions can worsen disc related pain.
- Injury: A sudden strain or trauma, such as lifting a heavy object or a fall, can damage the disc.
- Disc herniation: When the inner gel-like material of a disc leaks out, it can irritate nearby nerves and cause pain.
- Genetic factors: Some individuals may have a predisposition to early disc degeneration.
Common symptoms of discogenic pain
Discogenic pain is responsible for up to 40% of low back pain. The symptoms of discogenic pain can vary but often include:
- Localized pain: A deep, aching sensation in the lower back or neck that may worsen with sitting, bending, or twisting.
- Radiating pain: Pain that spreads to the hips, buttocks, thighs, or shoulders, depending on the affected area.
- Stiffness: Difficulty moving or maintaining certain positions for extended periods.
- Increased pain with activity: Pain may intensify during activities that put pressure on the spine.
Diagnosis of discogenic pain
Diagnosing discogenic pain involves evaluating your symptoms, medical history, and performing a physical examination. Discogenic low back pain often worsens with sitting, bending, or prolonged standing. Disc degeneration is part of the normal ageing process and most degenerate discs are not painful and should only be diagnosed as clinically relevant by a spinal specialist.
Imaging tests play a key role in diagnosis. These may include:
- MRI scans to assess disc health and identify signs of accelerated disc degeneration, Modic changes or annular tears.
- X-rays to evaluate spinal alignment, disc height and rule out other causes of pain.
Management of discogenic pain
Treatment for discogenic pain focuses on relieving symptoms and improving spine function. Options include:
- Physical therapy: Exercises to strengthen the core and back muscles, improve flexibility, and reduce strain on the spine is essential.
- Medications: Anti-inflammatory drugs and simple analgesics may help manage symptoms. Opiate medications are not recommended for discogenic pain.
- Lifestyle modifications: Maintaining a healthy body weight, practicing good posture, employing good lifting technique and avoiding activities that worsen the pain. In the gym, exercises such as dead lifts, squats, Olympic weights and rowing machine are known to improve muscle strength but can lead to disc injury.
- General exercise: Keeping fit with cardio exercise including walking, swimming and cycling.
- Injections: Corticosteroid injections can reduce inflammation and provide temporary pain relief and can assist rehabilitation exercises by providing a therapeutic window.
- Surgical intervention: In severe or persistent cases, surgery such as spinal fusion or disc replacement may be considered.

