Common Conditions
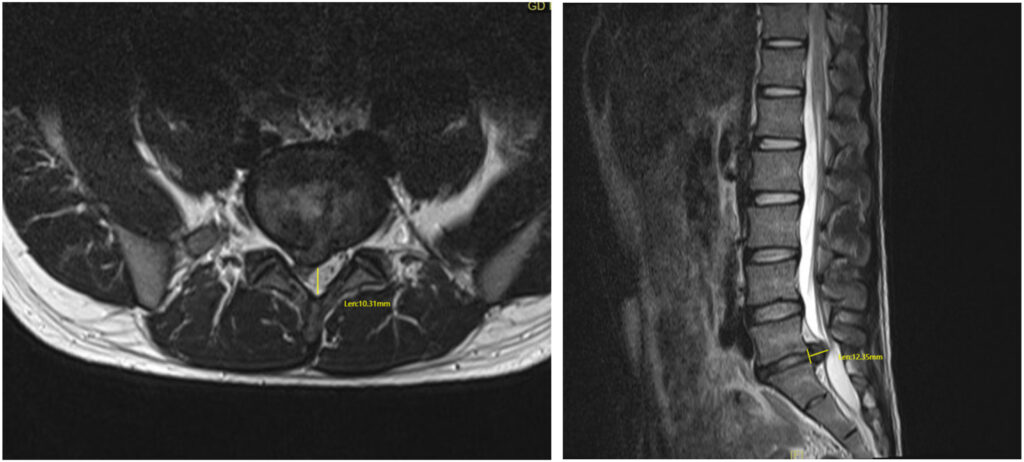
Disc Bulge (including protrusion/herniation)
A disc bulge occurs when one of the intervertebral discs extends broadly beyond its normal boundary of the adjacent vertebrae. Bulges are slightly different to protrusions or herniations, which are over a shorter area of the vertebra. When a disc bulges or protrudes, it can press on nearby nerves or occasionally the spinal cord, leading to spine pain or referred nerve symptoms. Disc bulges are extremely common even in healthy people and may affect the neck (cervical spine), mid back (thoracic spine), or lower back (lumbar spine). Most disc bulges are not relevant and don’t cause symptoms. Disc bulges are found in all age groups and are frequently reported on advance imaging (MRI and CT).
What causes a disc bulge?
A disc bulge can result from a variety of factors, including:
- Age-related changes: Over time, discs lose water content and elasticity, making them more prone to bulging. They are commonly reported on imaging in older people but this is usually a normal finding.
- Repetitive strain: Activities that involve frequent bending, twisting, or lifting can increase pressure on the discs. Also, annular tears can weaken a disc and lead to bulging or protrusion.
- Poor posture: Prolonged sitting, especially with poor ergonomics, can contribute to disc wear and tear.
- Injury or trauma: A fall, car accident, or sudden movement may cause a disc to acute bulge or protrusion.
- Heavy lifting: Lifting objects incorrectly or straining under load can put stress on the spine and weaken or damage a disc leading to bulging or protrusion.
Common symptoms of a disc bulge
Disc bulges are extremely common on radiology studies and cause anxiety. However, the majority do not cause any symptoms. However, if the bulge contacts or compresses nearby nerves, patients may experience:
- Localized pain: In the neck or back, depending on the location of the affected disc.
- Radiating pain: Pain that travels down the arms (if the cervical spine is affected) or legs (if the lumbar spine is affected).
- Numbness or tingling: In the limbs.
- Muscle weakness: In the arms or legs, if nerves are compressed.
- Stiffness: Reduced mobility or flexibility in the spine.
Diagnosis of a disc bulge
Only a spinal specialist should diagnose a clinically relevant disc bulge, based on clinical findings and imaging results as they are commonly reported on imaging. This will involve a detailed medical history, an examination and then assessment of radiological findings.
Imaging studies are often used to help in the diagnosis:
- MRI scans are the most effective tool for visualising disc bulges and assessing whether nearby nerves are being compressed or whether there are associated annular tears.
- CT scans are less useful and may ‘over-diagnose’ disc bulges.
X-rays are primarily used to rule out other causes of pain and can not accurately diagnose a disc bulge.
Management of a disc bulge
Treatment for a symptomatic disc bulge should always begin with conservative measures aimed at relieving symptoms. Some disc bulges and protrusions will resolve over time or with treatment, especially in healthier discs in younger people. These may include:
- Physical therapy: To strengthen spinal support muscles and improve posture.
- Medications: Anti-inflammatory drugs or simple analgesics to reduce discomfort.
- Epidural corticosteroid injections: In some cases, corticosteroid injections under CT guidance may help reduce disc and or nerve inflammation in the spine.
- Activity modification: Avoiding movements that aggravate symptoms and using proper lifting techniques.
- Surgical options: If symptoms are severe or don’t improve with other treatments, surgery may be considered to remove the bulging portion of the disc or relieve nerve compression (discectomy).

